A recent case illustrated the following:
"A recent pharmacy revenue audit discovered that 25-35% of the HCPCS (J-codes) in the pharmacy charge master were missing or invalid. This caused an estimated loss in pharmacy revenue of $10.5 million.” Source: Pharmacy Revenue Cycle Audits Can Bring Unexpected Returns; Miller, Fox-Smith hfma http://www.hfma.org/Content.aspx?id=3344
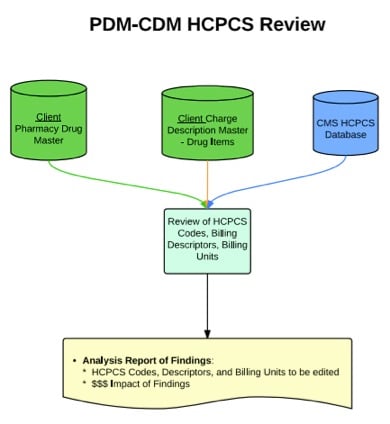
That's quite an alarming case study. The following workflow illustrates how your pharmacy can discover where the discrepancies are between the Pharmacy Drug Master (PDM) and the Charge Description Master (CDM).
The Pharmacy Drug Master (PDM) in the Pharmacy Information System (PIS) is the source of truth for the hospital's drug formulary. Any edits to the formulary must be updated in downstream systems. Updating the CDM with any applicable changes to the PDM is just as important from a financial integrity standpoint.
What steps can you take to ensure that the PDM and CDM are in sync?
CDM management is a team approach that involves the pharmacy, business office, patient financial services, health information management, IT, managed care, physicians, and other clinical departments. It's important that the pharmacy department is actively involved in ensuring that the drug (pharmacy) portion of the CDM is accurate. The following outline details the steps that a pharmacy can take to synchronize the PDM with the CDM.
- Extract PDM File:
- Extract detailed PDM file from the Pharmacy Information System.
- Review the following data fields: Package Info, Unit designation [in the case of Siemens pharmacy (GDU/GMOD)], Dispensing Info, Pricing, CDM description.
- Extract CDM File:
- Extract the pharmacy data from the CDM (contact the finance/business office to get this file).
- Review the following data fields: CDM number, Description, Unit, Price.
- Billing Description:
- Review the PDM and CDM billing description to ensure that there's a one-to-one match. (For example, both CDM and PDM description would read "Amoxicillin 500 mg cap.")
- HCPCS Codes and billing units:
- HCPCS Code – Healthcare Common Procedure Coding System (HCPCS) is maintained by the Centers for Medicare and Medicaid (CMS). These codes and billing units are updated throughout the year, so be sure to keep up with changes to the HCPCS codes impacting your organization. Refer to http://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/Alpha-Numeric-HCPCS.html for a drug list and quarterly updates. Drug HCPCS codes start with J or Q.
- Ensure that the J/Q code in the pharmacy PDM reflects the current HCPCS code for the drug and corresponds with the value for the drug in the CDM.
- HCPCS Billing Units - Each drug HCPCS code corresponds with a CMS billing unit.
- For example: (2014) Acetaminophen IV HCPCS Billing Unit = 10 mg. A standard dose of 1000 mg q6h equates to 100 HCPCS billing units. Ensure that the billed quantity is 100, not 1, to reflect accurate billing for the drug.
- Review the billing unit conversion (which can reside in the CDM or PDM, depending on your system) to ensure that it accurately reflects the current HCPCS value.
- HCPCS Code – Healthcare Common Procedure Coding System (HCPCS) is maintained by the Centers for Medicare and Medicaid (CMS). These codes and billing units are updated throughout the year, so be sure to keep up with changes to the HCPCS codes impacting your organization. Refer to http://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/Alpha-Numeric-HCPCS.html for a drug list and quarterly updates. Drug HCPCS codes start with J or Q.
- Note differences between the two files:
- If the description needs to be revised on the CDM, note what the revision would need to be on the Business Office side.
- Edit the pharmacy PDM as appropriate to reflect what’s in the CDM.
A full PDM-CDM review should be performed routinely. Many hospitals will conduct an annual review of these two files. Developing a PDM change-control process inclusive of requisite changes to the CDM streamlines the maintenance of the two systems. Identify key personnel (dedicated pharmacy and finance/business office personnel) to be responsible for the maintenance of this combined system. Having this system in place ensures accurate drug billing and financial integrity.


Comments